Human-Based Models for Rare Bone Diseases: A New Approach
An interdisciplinary research project on Osteogenesis imperfecta brings together clinical and laboratory expertise — with the goal of developing a human-relevant disease model and ultimately reducing animal testing.
How can cutting-edge lab technology help improve treatment for rare diseases like Osteogenesis imperfecta (OI)? In this project, researchers at the ETH Zurich are developing a human-based model to study how bone tissue forms in patients with OI — without relying on animal models. The close collaboration of the research team with the University Children’s Hospital Zurich plays a key role, enabling access to patient-derived cells and clinical expertise.
In the following interview, project leader Xiao-Hua Qin, and his doctoral student Doris Zauchner share insights into the progress so far, current challenges, and the potential of this new technology.
As part of your project, you are collaborating with the University Children's Hospital Zurich. How does this partnership contribute to the development of the project?
This partnership actually began even before the official start of the NRP 79 project, initialized by Professor Ralph Müller. Over the years, our collaboration with the University Children's Hospital Zurich has developed into a strong, trust-based relationship, driven not only by scientific interest but also by a shared desire to translate research into something that can directly benefit patients.
It’s a truly synergistic partnership. On the one hand, we rely on the hospital for access to patient-derived material and clinical expertise. On the other hand, we are developing technologies in our lab that could potentially be used in the hospital setting in the future – for example, in diagnosis or treatment decision-making.
We’ve also collaborated in supervising students together, enabling valuable knowledge transfer. For example, students from both institutions have worked in each other’s labs. This has helped us to better understand the complexity of the disease and to integrate clinical and technical perspectives.
In short, without this partnership, the project would not be possible in its current form.
How many children worldwide are affected by OI, and what is the situation in Switzerland? Are these numbers increasing or decreasing?
OI is a rare genetic disorder, and as with many genetic diseases, the prevalence does not change significantly over time. Globally, it affects about 1 in 15,000 people. In Switzerland, approximately 400 individuals live with OI.
3RCC Young Investigator Award
Doris Zauchner, who is part of the project team, was recently honored with the 3RCC Young Investigator Award for her innovative work on human-relevant bone disease models.
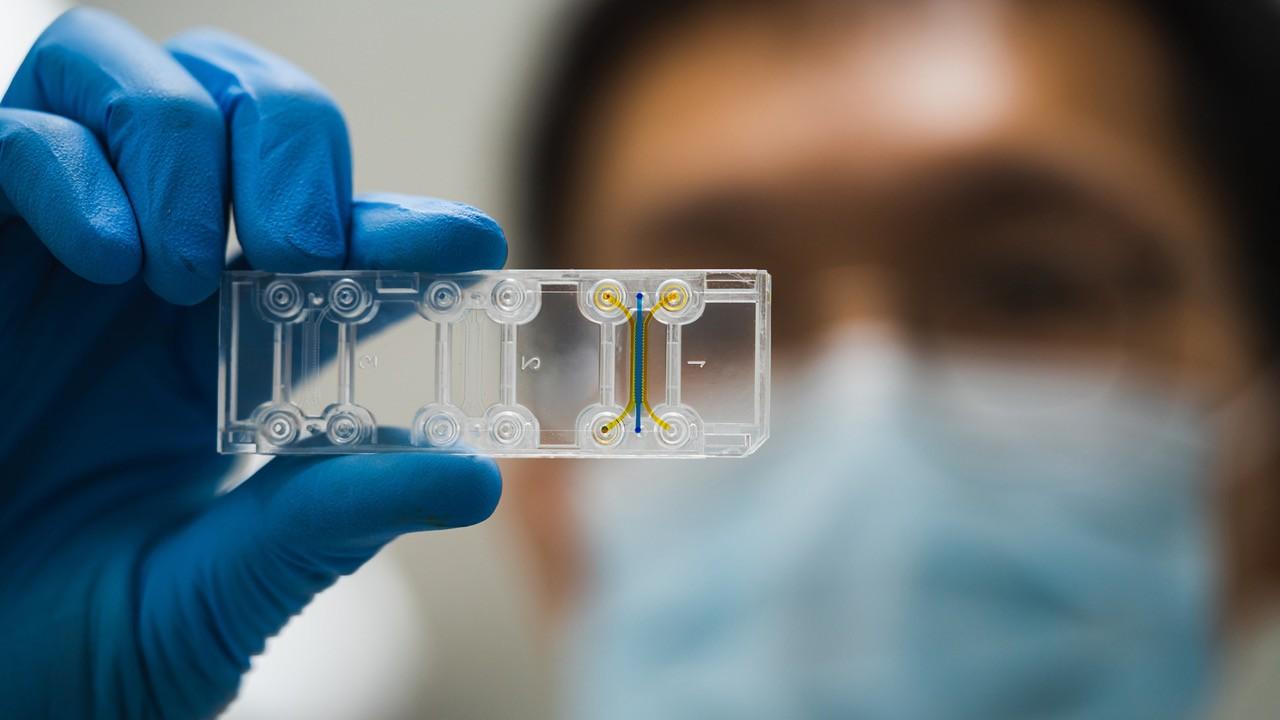
“With our bone-on-chip model, we aim to develop a human-relevant alternative to animal testing that deepens our understanding of brittle bone disease and opens paths toward personalized treatments", says Zauchner. "I hope that approaches like this will advance rare disease research while reducing the need for animal experiments. Being awarded the 3RCC Young 3Rs Investigator Award is both an honor and an encouragement for me to continue developing more ethical and human-relevant research tools."
What role does direct patient feedback play in clinical trials? How does this feed into the further development of your model and therapeutic approaches?
Currently, our work is still in the early research and development phase. We are focused on developing and refining the technology in the lab, and have not yet reached the stage where we are working directly with patients or conducting clinical trials.
That said, our clinical partners at the University Children’s Hospital are in close contact with patients and handle all interactions under strict ethical regulations. We work under an approved Material Transfer Agreement, which allows us to receive patient-derived cells for research purposes, based on ethical clearance.
Our long-term goal is to help make personalized treatments for OI patients. Since OI affects each patient differently, it's important to understand how their individual cells behave. If our technology proves successful, doctors could one day use a patient’s own cells to predict how well a specific treatment might work. This approach is part of the growing movement in research towards personalized medicine and patient-specific models.
What progress has been made so far with the bone cell model in the laboratory? What are the biggest challenges?
Our initial focus was on developing the biomaterial in which bone cells can be embedded. We first established the model using healthy donor cells from commercial sources and demonstrated that it functions well in microfluidic organ-on-chip systems. This work has already been published.
In a second step, we began incorporating patient-derived cells into the model. For example, in an actual study, we are comparing specific proteins from a OI-patient to that of a healthy donor. This helps us to identify disease-specific differences in bone tissue formation.
One major challenge we face is sourcing healthy control cells. While patient material is available, often as surgical waste from routine procedures, it is ethically difficult to collect tissue from healthy children. As a result, we have very limited access to healthy donor cells.
What potential do you see in expanding the organoid-on-a-chip model for research into other bone diseases such as osteoporosis or bone tumours?
The potential is very high. The same materials and technologies we are developing for OI have already shown promise in other areas of bone research. For example, bone diseases such as osteoporosis could benefit greatly from such personalized models, as could conditions like bone tumors or other musculoskeletal diseases.
We are also exploring applications in muscle diseases and metabolic conditions like diabetes and obesity, which increasingly affect musculoskeletal health. This makes the platform a promising candidate for broader biomedical research, not only within rare diseases but also in more common, population-wide conditions.
What next steps, for example with regard to implementation, are planned for the project in the coming years?
In the coming phase, we are focusing on deepening the characterization of our bone cell model. We have initiated new collaborations within the NRP 79 network, particularly with a group in Fribourg that specializes in analyzing protein expression and quality. This is a complementary skillset that will help us further validate the model.
We also plan to begin testing drug treatments in the model. One proposal is to investigate hormone-based therapies, as these may influence bone development and matrix production. Our focus remains on fundamental research at this stage, but everything is geared towards building a solid foundation for future clinical translation.